|
Female children/Female adolescents/Women of childbearing potential/Pregnancy: Valproate should not be used in female children, in female adolescents, in women of childbearing potential and pregnant women unless alternative treatments are ineffective or not tolerated because of its high teratogenic potential and risk of developmental disorders in infants exposed in utero to valproate. The benefit and risk should be carefully reconsidered at regular treatment reviews, at puberty and urgently when a woman of childbearing potential treated with valproate plans a pregnancy or if she becomes pregnant. Women of childbearing potential must use effective contraception during treatment and be informed of the risks associated with the use of valproate during pregnancy. In women planning to become pregnant all efforts should be made to switch to appropriate alternative treatment prior to conception, if possible. Valproate therapy should only be continued after a reassessment of the benefits and risks of the treatment with valproate for the patient by a physician experienced in the management of epilepsy. |
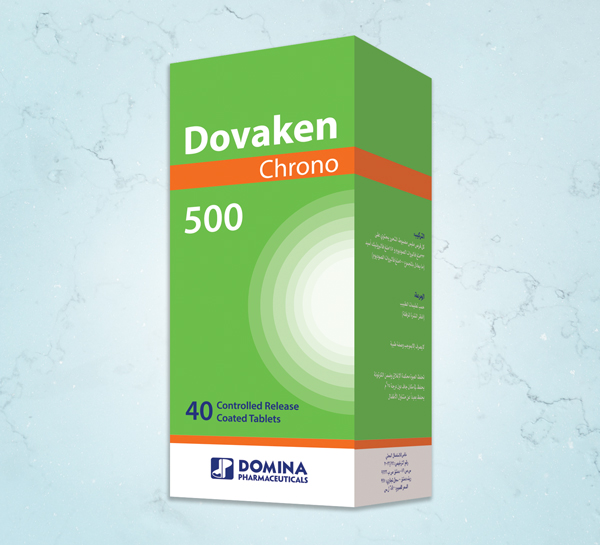
COMPOSITION:
Each controlled release coated tablet contains 333mg sodium valproate and 145mg valproic acid equivalent to 500mg sodium valproate –
MECHANISM OF ACTION:
Sodium valproate is an anticonvulsant.
- The most likely mode of( Controlled Release Coated Tablets) for valproate is potentiation of the inhibitory action of gamma amino-butyric acid (GABA) through an action on the further synthesis or further metabolism of GABA.
PHARMACOKINETICS:
The half-life of sodium valproate is usually within the range 8-20 hours. It is usually shorter in children.
In patients with severe renal insufficiency it may be necessary to alter dosage in accordance with free plasma valproic acid levels.
The effective therapeutic range for plasma valproic acid levels is 40-100mg/litre. The percentage of free (unbound) drug is usually between 6% and 15% of the total plasma levels. An increased incidence of adverse effects may occur with plasma levels above the effective therapeutic range.
INDICATIONS:
Epilepsy: Primary generalized epilepsy (petit mall absences, various forms of myoclonic and tonic clonic grand mall seizures) Partial (focal) epilepsy either alone or as adjuvant therapy
Mania: For the treatment of Mania where other therapy has proved inadequate or is inappropriate.
CONTRAINDICATIONS:
- Pregnancy
- Pre-existing chronic or acute hepatic dysfunction or family history of severe hepatitis, particularly medicine related.
- Known hypersensitivity to sodium valproate.
- Known urea Cycle disorders
- Known hepatic porphyria
- Valproate is contraindicated in patients known to have mitochondrial disorders caused by mutations in the nuclear gene encoding the mitochondrial enzyme polymerase γ (POLG), e.g. Alpers-Huttenlocher Syndrome, and in children under two years of age who are suspected of having a POLG-related disorder.
WARNINGS AND PRECAUTIONS:
Look at box warning.
Patients with known or suspected mitochondrial disease:
Valproate may trigger or worsen clinical signs of underlying mitochondrial diseases caused by mutations of mitochondrial DNA as well as the nuclear encoded POLG gene. In particular, valproate-induced acute liver failure and liver-related deaths have been reported at a higher rate in patients with hereditary neurometabolic syndromes caused by mutations in the gene for the mitochondrial enzyme polymerase γ (POLG), e.g. Alpers-Huttenlocher Syndrome.
Pancreatitis: Some cases have occurred shortly after initial use while others have occurred after several years children are at particular risk but this risk decreases with increasing age.
Severe seizures, neurological impairment or anticonvulsant therapy may be risk factors.
Hepatic failure with pancreatitis increases the risk of fatal outcome.
Patients and guardians should be warned that acute abdominal pain nausea. Vomiting and /or anorexia can be symptoms of pancreatitis that require prompt medical attention .If pancreatitis is diagnosed sodium valproate should be discontinued and alternative treatment initiated.
Hepatic dysfunction: Hepatic failure resulting in fatalities has occurred in patients whose treatment included valproic acid or sodium Valproate. Patients most at risk are children ,particularly those under the age of 3 years and those with congenital metabolic or degenerative disorders, organic brain disease or severe seizure disorders associated with mental retardation.
Usually occurred during the first six months of therapy, the period of maximum risk being 2 to12 weeks, and usually involved multiple anticonvulsant therapy. Mono-therapy is to be preferred in this group of patients.
Clinical symptoms are usually more helpful than laboratory investigations in the early stages of hepatic failure. Serious or fatal hepatotoxicity may be preceded by nonspecific symptoms usually of sudden onset such as loss of seizure control, malaise, weakness, lethargy, facial edema; anorexia ,vomiting, abdominal pain, drowsiness ,jaundice. These are an indication for immediate -withdrawal of the medicine. Patients should be monitored closely for the appearance of these symptoms and should be instructed to report any such signs to the clinician for investigation when they occur.
Raised liver enzymes: are not uncommon during treatment with sodium valproate particularly if used in conjunction with other anticonvulsants, and are usually transient of respond to dosage reduction. Patients with such biochemica1 abnormalities should be reassessed clinically and tests of liver function should be monitored more frequently. An abnormally low prothrombin rate; particularly in association with other relevant abnormalities(significant decrease in fibrinogen and coagulation factors; increased bilirubin level and raised transaminases) requires cessation of treatment and the substitution of alternative medicines to avoid precipitating convulsions. Any concomitant use of salicylates should be stopped, since they employ the same metabolic pathway.
Impaired renal function: Lower doses may be required since free drug levels may be high owing to lowered serum albumin and poor urinary excretion of free drug metabolites. As monitoring of plasma concentrations may be misleading dosage should be adjusted according to clinical monitoring.
Lupus erythematous:Although immune disorders have been noted only exceptionally during the use of sodium valproate the potential benefit of sodium valproate should be weighed against its potential risk in patients with systemic lupus erythematous.
Hyperammonaemia: When urea cycle enzymatic deficiency is suspected metabolic investigations should be performed prior to treatment because of the risk of Hyperammonaemia with valproate. Hyperammonaemia, which may be present in the absence of abnormal liver function tests, can occur in patients during treatment with sodium valproate. This may occasionally present clinically, with or without lethargy or coma, with symptoms such as vomiting, ataxia and increasing clouding of consciousness. Should these symptoms occur, Hyperammonaemia encephalopathy should be considered and drug should be discontinued.
Urea Cycle Disorders (UCD): Hyperammonaemic encephalopathy, sometimes fatal, has been reported following initiation of valproate therapy in patients with urea cycle disorders,which is a group of uncommon genetic abnormalities, particularly ornithine transcarbamylase deficiency. Prior to the initiation of valproate therapy, evaluation for UCD should be considered in the following patients:
1) Those with a history of unexplained encephalopathy or coma, encephalopathy associated with a protein load, pregnancy-related or postpartum encephalopathy, unexplained mental retardation, or history of elevated plasma ammonia or glutamine;
2) Those with cyclical vomiting and lethargy, episodic extreme irritability, ataxia, low BUN, or protein avoidance;
3) Those with a family history of UCD or a family history of unexplained infant deaths (particularly males);
4) Those with other signs or symptoms of UCD.
Patients who develop symptoms of unexplained hyperammonaemic encephalopathy while receiving valproate therapy should receive prompt treatment (including discontinuation of valproate therapy) and be evaluated for underlying urea cycle disorders.
Ornithine Transcarbamylase (OTC) Deficiency: Females may show a range of symptoms due to Hyperammonaemia which, may be episodic, and therefore difficult to diagnose. The acute symptoms include headaches, vomiting, irritability, bizarre behavior, lethargy, ataxia, tremors, seizures (generalized tonic-clonic or focal) and coma. Valproate may precipitate Hyperammonaemia symptoms in those who have pre-existing OTC deficiency. As the symptoms may include seizures, any female with valproate-associated symptomatic Hyperammonaemia should be evaluated for OTC deficiency. Investigations should include measurement of plasma amino acids and the immediate cessation of valproate should result in clinical improvement.
Surgery: Prolongation of bleeding time, sometimes with thrombocytopenia, has occurred with sodium valproate therapy. Platelet function should be monitored before surgery is undertaken in patients receiving sodium valproate.
Other: Blood tests (blood cell count, including platelet count, bleeding time and coagulation tests) are recommended prior to initiation of therapy, and in case of spontaneous bruising or bleeding.
Suicidal Behavior and Ideation: Antiepileptic drugs, including sodium valproate increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Abrupt withdrawal: The possible risk of fits after sudden cessation of sodium valproate should be borne in mind. If it is the only anticonvulsant used and has to be withdrawn for more than 12 hours because of surgery, control of epilepsy may be lost.
Carbapenem antibiotics: The concomitant use of sodium valproate and carbapenem antibiotics is not recommended.
Check the following before use:
-Thrombocytopenia: Platelet counts and coagulation tests are recommended before initiating therapy and at periodic intervals
-Ornithine transcarbamylase (OTC) deficiency: A familial history of infant mortality or patient history of OTC deficiency or of seizures or coma in the presence of mental retardation suggests the need to exclude OTC deficiency .
Weight gain: patients should be warned of the risk of weight gain at the initiation of the therapy and appropriate strategies should be adopted to minimize the risk.
USE IN PREGNANCY ( CATEGORY D ) :
During pregnancy, maternal tonic- clonic seizures and status epilepticus with hypoxia carry a particular risk of death for mother and for the unborn child. The risk of a mother with epilepsy giving birth to a baby with an abnormality is about three times that of the normal population. The following recommendation should be taken into consideration: This medicine should not be used during pregnancy and in women of child-bearing potential unless clearly necessary, that is, in situations where other treatments are ineffective or not tolerated. This assessment is to be made before sodium valproate is prescribed for the first time, or when a woman of child-bearing potential treated with sodium valproate plans a pregnancy. Women of child-bearing potential must use effective contraception during treatment.
It is recommended that: • Women on antiepileptic drugs (AEDs) receive pre-pregnancy counselling with regard to the risk of foetal abnormalities;
• AEDs should be continued during pregnancy and monotherapy should be used if possible at the lowest effective dose as risk of abnormality is greater in women taking combined medication;
• If appropriate, folic acid supplementation (5mg) should be commenced four weeks prior to and continue for twelve weeks after conception;
• Specialist prenatal diagnosis including detailed mid-trimester ultrasound should be offered.
USE IN LACTATION:
Valproate is excreted in breast milk. Concentrations in breast milk have been reported to be 1 to 10% of serum concentration. It is not known what effect this would have on a breast-fed infant. As a general rule, breastfeeding should not be undertaken whilst a patient is receiving sodium valproate.
Pediatric Use:
The potential benefit of the drug should be weighed against the risk of pancreatitis or liver damage in such patients prior to initiation of therapy. The concomitant use of salicylates should be avoided in children under 3years of age due to the risk of liver toxicity and the concomitant use of barbiturates may require dosage adjustment. Monotherapy is recommended in children under 3 years of age, when prescribing sodium valproate. Young children are at particular risk for pancreatitis, however this risk decreases with increasing age.
Effect on Ability to Drive or Operate Machinery Patients should be warned of the risk of transient drowsiness, especially in cases of anticonvulsant polytherapy, too high a starting dose, too rapid a dose escalation or association with benzodiazepines.
INTERACTIONS WITH OTHER MEDICINES:
Effects of sodium valproate on other medicines:
Alcohol: Valproic acid may potentiate the CNS depressant activity of alcohol.
Carbamazepine: Valproate may displace carbamazepine from protein binding sites and may inhibit the metabolism of both carbamazepine and its metabolite carbamazepine 10. 11 epoxide and consequently potentiate toxic effects of carbamazepine. Clinical monitoring is recommended especially at the beginning of combined therapy with dosage adjustment when appropriate.
Lamotrigine: sodium valproate reduces lamotrigine metabolism and increases its mean half-life, this interaction may lead to increase lamotrigine toxicity. In particular serious skin rashes. Clinical monitoring is recommended and lamotrigine dosage should be decreased as appropriate.
Phenobarbitone: Sodium valproate may block the metabolism of barbiturates causing an increase in phenobarbitone plasma levels, which, particularly in children, may, be associated with sedation. Combination of sodium valproate and phenobarbitone can cause .CNS depression without significant elevation of serum level of either drug. Therefore, clinical monitoring is recommended throughout the first 15 days of combined treatment. A reduction in the dose of phenobarbitone and/or valproate may be necessary and this should also be borne in mind if medicines which are metabolized to phenobarbitone (e.g. primidone, methylphenobarbitone) are given with sodium valproate.
Phenytoin: There have been reports of breakthrough seizures occurring with the combination of sodium valproate and phenytoin. Most reports have noted a decrease in total plasma phenytoin concentration. An initial fall in total phenytoin levels with subsequent increase in phenytoin levels has also been reported. The dosage of phenytoin may require adjustment when given in conjunction with valproate as required by the clinical situation.
Medicines with extensive protein binding: The concomitant administration of sodium valproate with medicines that exhibit extensive protein binding (e.g. aspirin, carbamazepine, phenytoin, and warfarin) may result in alteration of serum drug levels.
Anticoagulants: The effect of sodium valproate on anticoagulants which modify platelet function is unknown. Caution is recommended when administering anticoagulants and other products which have anticoagulant properties (e.g. warfarin and aspirin).
Ethosuximide: The interaction between ethosuximide and valproate is not normally of clinical significance. There is evidence that sodium valproate may inhibit ethosuximide metabolism, especially in the presence of other anticonvulsants. Patients receiving this combination should be monitored clinically.
Oral contraceptives: The enzyme inducing effect of valproate is appreciably less than that of certain other anticonvulsants and loss of efficacy of oral contraceptive agents does not appear to be a problem.
Psychotropic agents:Sodium valproate may potentiate the effects of MAOIs, neuroleptics, benzodiazepines and other antidepressants, and the dose of these medicines should be reduced accordingly.
Clonazepam: The concomitant use of sodium valproate and clonazepam may produce absence status.
Clozapine: Caution is advised during concomitant administration as competitive protein binding may potentiate an increase in clozapine or valproate levels.
Diazepam: Sodium valproate displaces diazepam from its plasma binding sites and inhibits its metabolism. Monitoring of free diazepam levels may be necessary if the patient becomes sedated.
Lorazepam: A decrease in lorazepam plasma clearance may occur with concomitant administration of sodium valproate.
Midazolam: Free plasma midazolam may increase in patients receiving valproate. Potentially leading to an increase of the midazolam response.
Primidone: Valproate increases primidone plasma levels with exacerbation of its adverse effects (such as sedation); these signs cease with long-term treatment. Clinical monitoring is recommended especially at the beginning of combined therapy with dosage adjustment when appropriate.
Zidovudine: Valproate may raise zidovudine plasma concentrations leading to increased zidovudine toxicity.
Tricyclic antidepressants: Sodium valproate may inhibit the metabolism of tricyclic antidepressants. Clinical monitoring of free antidepressant levels may be necessary.
Other medicines: There was no notable interaction between valproate and lithium.
Effects of other medicines on valproate:
Aspirin: concomitant administration of sodium valproate and aspirin may result in displacement of valproate from protein sites, resulting in a rise in free levels in addition. Aspirin appears to inhibit the metabolism of valproate. Thus caution is advisable when patients on sodium valproate are prescribed aspirin. Furthermore patients requiring long-term aspirin therapy may require a reduction in dosage of sodium valproate.
Felbamate: Felbamate may increase valproate serum concentrations. Valproate dosage should be monitored when given in combination with felbamate. Valproic acid may decrease the felbamate mean clearance.
Phenobarbitone, Phenytoin and Carbamazepine: These medicines can decrease steady-state valproate levels in patients by increasing the intrinsic clearance of valproate. Dosages should be adjusted according to clinical response and blood levels in case of combined therapy.
Antidepressants: Antidepressants (including MAOIs, tricyclic antidepressants and SSRIs) may have the potential to inhibit the metabolism of valproate via the cytochrome P450 system. However, there is not expected to be any significant interaction within normal therapeutic doses. Antidepressants can lower the seizure threshold of non-stabilized epileptic patients, and so careful and regular monitoring of their condition is indicated.
Clozapine: Caution is advised during concomitant administration as competitive protein binding may potentiate an increase in clozapine or valproate levels.
Chlorpromazine: Chlorpromazine may inhibit the metabolism of valproate.
Fluoxetine: Fluoxetine may inhibit the metabolism of valproate as it does with tricyclic antidepressants, carbamazepine and diazepam.
Mefloquine: Mefloquine increases valproic acid metabolism and has a convulsing effect; therefore epileptic seizures may occur in cases of combined therapy.
Cimetidine or Erythromycin: Valproate serum levels may be increased (as a result of reduced hepatic metabolism) in case of concomitant use with cimetidine or erythromycin.
Carbapenem antibiotics: Decrease in valproate blood level sometimes associated with convulsions has been observed when valproate and carbapenem antibiotics (panipenem, meropenem, imipenem, ertapenem, biapenem) were combined. Due to the rapid onset and the extent of the decrease, co-administration of carbapenem antibiotics in patients stabilised on valproic acid should be avoided. If treatment with these antibiotics cannot be avoided, close monitoring of valproate blood level should be performed.
Vitamin K dependent factor anticoagulant: Close monitoring of prothrombin rate should be performed in case of concomitant use of vitamin K dependent factor anticoagulant.
Rifampicin: Rifampicin may decrease the valproate blood levels resulting in a lack of therapeutic effect. Therefore, valproate dosage adjustment may be necessary when it is co-administered with rifampicin.
Other interactions:
Topiramate: Concomitant administration of valproate and topiramate has been associated with encephalopathy and/or hyperammonaemia. Patients treated with those two drugs should be carefully monitored for signs and symptoms of hyperammonaemic encephalopathy.
ADVERSE EFFECTS:
Skin and subcutaneous tissue disorders: Transient increase in hair loss has been observed. Dermatological reactions consistent with immune adverse reactions such as pruritus, rash, urticaria, Stevens Johnson Syndrome have been noted.
Reproductive system and breast disorders: There have been reports of irregular menses and secondary amenorrhoea and rare cases of breast enlargement and galactorrhoea. There have been reports of male infertility.
Gastrointestinal disorders: Nausea, vomiting, abdominal cramp, upper abdominal pain, anorexia, increased appetite and diarrhoea are usually transient and rarely require discontinuation of therapy or limitation of dose.
Blood and lymphatic system disorders: Valproic acid inhibits the second stage of platelet aggregation.Reversible prolongation of bleeding time have been reported but have usually been associated with doses above those recommended. Frequent occurrence of thrombocytopaenia, rare cases of pancytopaenia without bone marrow depression. Isolated cases of decreased blood fibrinogen and prolonged prothrombin time have been reported.
Anemia, red cell hypoplasia, neutropenia and leucopenia have also been reported. In most cases the blood picture returned to normal when medicine was discontinued.Bone marrow failure, including pure red cell aplasia and agranulocytosis have been reported.
Hepatobiliary disorders: Hepatic dysfunction, including hepatic failure resulting, in fatalities, has occurred in patients whose treatment included valproic acid or sodium valproate.
Metabolism and nutrition disorders: Hyperammonaemia has been reported in association with valproate therapy and may be present despite normal liver function tests. Asymptomatic elevations of ammonia are more common and, when present, require close monitoring of plasma ammonia levels. If the elevation is significant (above 3N) and persists, discontinuation of valproate therapy should be considered. Very rare cases of hyponatremia have been reported. Syndrome of Inappropriate Secretion of ADH (SIADH) has been reported.
Nervous system disorders: The true incidence of drowsiness and sedation with sodium valproate is difficult to assess, as mostly it was administered in combination with other medicines sodium valproate however, may have an intrinsic sedative action in addition to potentiating sedative effects of other anticonvulsants (e.g. barbiturates, clonazepam) and CNS depressants, including alcohol. Uncommon cases of ataxia have been reported. Headache, nystagmus, diplopia, tremor, dizziness, depression, hallucinations and coma have occurred rarely and usually in association with other anticonvulsants. Excitement, hyperactivity, aggression and behavioural disorders have been rarely reported, usually in children at the start of treatment. Stupor, either isolated or in conjunction with recurrence of seizures, may occur and is most often associated with polytherapy, too high a starting dose or too rapid a dose escalation. Rare cases of lethargy and confusion. Very rare cases of reversible dementia associated with reversible cerebral atrophy have been reported. Extrapyramidal disorder which may not be reversible, including reversible Parkinsonism has been reported.
Ear and labyrinth disorders: Deafness, either reversible or irreversible, has been reported rarely.
Immune system disorders: Angioedema, Drug Rash with Eosinophilia and Systemic Symptoms (DRESS) syndrome and allergic reactions have been observed.
Renal and urinary disorders: Very rare cases of enuresis have been reported. There have been isolated reports of a reversible Fanconi's syndrome associated with valproate therapy.
Vascular disorders: The occurrence of vasculitis has been reported.
General disorders: Oedema has been reported. Increase in appetite and weight may occur. Since it is a risk factor for polycystic ovary syndrome, it should be carefully monitored.
DOSAGE AND ADMINISTRATION:
Sodium valproate E.C.tablets may be given twice daily.
Sodium valproate Oral Solution should be given in divided doses. Should not be diluted.
Sodium valproate should preferably be taken with or after food: the enteric-coated tablet must be swallowed whole, if necessary with a little water.
Sodium valproate 500 mg E.C.tablets is recommended for patients requiring high doses. Sodium valproate may take several days to show an initial effect and in some cases may take from 2 to 6 weeks to exhibit its maximum effect.
Epilepsy
Monotherapy:
Adults : Dosage should start with 600 mg daily increasing by 200mg/day at three-day intervals until control is achieved. This is generally within the range 1000 to 2000 mg/day.(i.e. 20 to 30 mg/kg/day) where adequate control is not achieved within this range the dose may be further increased to 2500 mg/day.
Children >20 Kg: The starting dose is 400 mg/day (regardless of weight) and increased at time intervals until control is achieved. This is generally within the range 20-30 mg/kg/day.
Children <20Kg: 20 mg/kg/day, and in severe cases this may be increased but only in patients in whom plasma Valproic acid levels can be monitored. Above 40 mg/kg/day, clinical chemistry and hematological parameters should be monitored.
General considerations: Optimum dosage is mainly determined by seizure control and routine measurement of plasma levels is unnecessary.
Combined therapy:
In certain cases it may be necessary to raise the dose by 5 to 10 mg/kg/day when used in combination with anticonvulsants which induce liver enzyme activity, e.g. phenytoin, phenobarbitone and carbamazepine.
Mania
Initially dosage should start with 600 mg daily increasing by 200 mg/day at three-day intervals until control is achieved. This is generally within the range 1,000 to 2,000 mg/day, (i.e. 20 to 30 mg/kg/day). Where adequate control is not achieved within this range the dose may be further increased to 2,500 mg/day.
Impaired renal function: Lower doses may be required since free drug levels may be high owing to lowered serum albumin and poor urinary excretion of free drug metabolites.
OVERDOSAGE :
Cases of accidental and suicidal overdosage have been reported. Fatalities are rare.
Symptoms: May include serious CNS depression and impairment of respiration. In cases of overdose, long half-lives up to 30 hours have been reported. Signs of an acute massive overdose usually include coma, with muscular hypotonia, hyporeflexia and miosis, impaired respiratory functions and metabolic acidosis. Symptoms may however be variable and seizures have been reported in the presence of very high plasma levels. Cases of intracranial hypertension related to cerebral edema have been reported. Deaths have occurred following massive overdose; nevertheless, a favorable outcome is usual.
Treatment:
Establish airway and breathing and evaluate circulatory status. Assisted mechanical ventilation may be required in cases of respiratory depression. Activated charcoal may reduce the absorption of the medicine if given within one or two hours after ingestion. In patients who are not fully conscious or have impaired gag reflex, consideration should be given to administering activated charcoal via nasogastric tube, once the airway is protected. Hemodialysis and hemoperfusion have been used successfully. Intravenous naloxone has also been used sometimes in association with activated charcoal given orally. Provided that adequate supportive treatment is given, full recovery usually occurs. Particular attention should be given to the maintenance of an adequate urinary output. Hepatic and pancreatic function should be monitored.