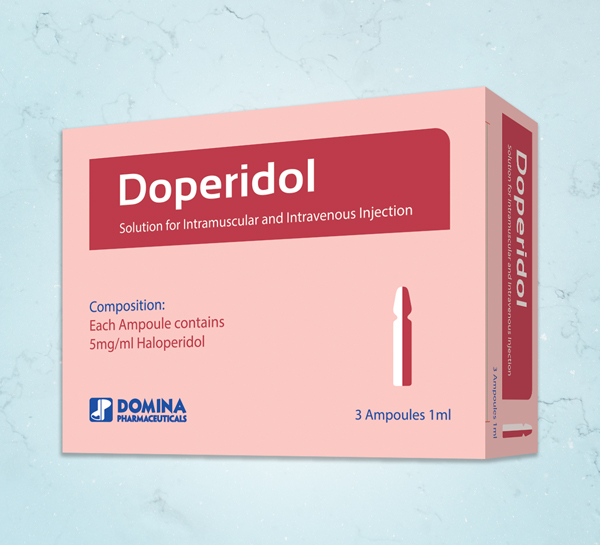
COMPOSITION:
Each 1ml Solution for injection contains 5mg Haloperidol.
MECHANISM OF ACTION:
Haloperidol is an antipsychotic belonging to the butyrophenones group. It is a potent central dopamine type 2 receptor antagonist, and at recommended doses, has low alpha-1 antiadrenergic activity and no antihistaminergic or anticholinergic activity.
INDICATIONS:
- Rapid control of severe acute psychomotor agitation associated with psychotic disorder or manic episodes of bipolar I disorder when oral therapy is not appropriate.
- Acute treatment of delirium when non-pharmacological treatments have failed.
- Treatment of mild to moderate chorea in Huntington's disease, when other medicinal products are ineffective or not tolerated, and oral therapy is not appropriate.
- Postoperative nausea and vomiting.
DOSAGE AND ADMINISTRATION:
Adults:
A low initial dose is recommended and this must be adjusted according to the patient's response in order to determine the minimal effective dose .
Haloperidol dose recommendations for adults aged 18 years and above:
1- Rapid control of severe acute psychomotor agitation associated with psychotic disorder or manic episodes of bipolar I disorder when oral therapy is not appropriate:
• 5 mg intramuscularly.
• May be repeated hourly until sufficient symptom control is achieved.
• In the majority of patients, doses up to 15 mg/day are sufficient. The maximum dose is 20 mg/day.
• The continued use of haloperidol should be evaluated early in treatment . Treatment with haloperidol solution for injection must be discontinued as soon as clinically indicated and, if further treatment is needed, oral haloperidol should be initiated at a 1:1 dose conversion rate followed by dose adjustment according to clinical response.
2- Acute treatment of delirium when non-pharmacological treatments have failed:
•1 to 10 mg intramuscularly.
• Treatment should be started at the lowest possible dose, and the dose should be adjusted in increments at 2- to 4 hour intervals if agitation continues, up to a maximum of 10 mg/day.
3- Treatment of mild to moderate chorea in Huntington's disease, when other medicinal products are ineffective or not tolerated, and oral therapy is not appropriate:
• 2 to 5 mg intramuscularly.
• May be repeated hourly until sufficient symptom control is achieved or up to a maximum of 10 mg/day.
4- Single or combination prophylaxis in patients at moderate to high risk of postoperative nausea and vomiting, when other medicinal products are ineffective or not tolerated:
• 1 to 2 mg intramuscularly, at induction or 30 minutes before the end of anaesthesia.
5- Combination treatment of postoperative nausea and vomiting when other medicinal products are ineffective or not tolerated:
• 1 to 2 mg intramuscularly.
Treatment withdrawal:
Gradual withdrawal of haloperidol is advisable
Elderly:
The recommended initial haloperidol dose in elderly patients is half the lowest adult dose according to the patient's response.
The maximum dose is 5 mg/day.
Renal impairment: No dose adjustment is recommended, but caution is advised when treating patients with renal impairment.
Hepatic impairment: Since haloperidol is extensively metabolised in the liver, it is recommended to halve the initial dose. Further doses may be administered and adjusted according to the patient's response.
Children under 18 years and adolescents: the safety has not been established.
CONTRAINDICATIONS:
- Hypersensitivity to the active substance or to any of the excipients.
- Comatose state.
- Central nervous system (CNS) depression.
- Parkinson's disease.
- Dementia with Lewy bodies.
Progressive supranuclear palsy.
• Known QTc interval prolongation or congenital long QT syndrome.
- Recent and Uncompensated acute myocardial infarction.
- Uncompensated heart failure.
- History of ventricular arrhythmia.
- Uncorrected hypokalaemia.
- Concomitant treatment with medicinal products that prolong the QT interval
SIDE EFFECTS:
- Very Common (≥ 1/10): Agitation, Insomnia, extrapyramidal disorder, hyperkinesias, headache.
- Common (≥ 1/100 to < 1/10): Depression, psychotic disorder, tardive dyskinesia, oculogyric crisis, dystonia, dyskinesia, akathisia, bradykinesia, hypokinesia, hypertonia, somnolence, tremor, dizziness, visual disturbance, orthostatic hypotension, hypotension, constipation, dry mouth, salivary hypersecretion, nausea, vomiting, liver function test abnormal, rash, urinary retention, erectile dysfunction, weight increased/decreased.
- Uncommon: Leukopenia, Hypersensitivity, Confusional state; Libido Decreased; Loss of libido; Restlessness, Convulsion; Parkinsonism; Sedation; Muscle Contractions Involuntary, Vision blurred, Tachycardia, Dyspnoea. Hepatitis jaundice , photosensitivity reaction , urticaria, pruritus , hyperthidrosis ,torticollis , muscle rigidity or spasm ,musculoskeletal stiffness ,amenorrhoea , dysmenorrhoea , galactorrhoea breast , discomfort , breast pain ,gait disturbance , hyperthermia oedema.
PRECAUTIONS:
1- Increased mortality in elderly people with dementia: Rare cases of sudden death have been reported in psychiatric patients receiving antipsychotics, including haloperidol
2- Elderly patients with dementia-related psychosis treated with antipsychotics are at an increased risk of death. Analyses of seventeen placebo-controlled studies (modal duration of 10 weeks), largely in patients taking atypical antipsychotics, revealed a risk of death in treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10 week controlled study, the rate of death in patients treated with antipsychotics was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that treatment of elderly patients with haloperidol is also associated with increased mortality. This association may be stronger for haloperidol than for atypical antipsychotic medicinal products, is most pronounced in the first 30 days after the start of treatment, and persists for at least 6 months.
3- Haloperidol solution for injection is not indicated for the treatment of dementia-related behavioural disturbances.
Cardiovascular effects:
- QTc prolongation and/or ventricular arrhythmias, in addition to sudden death, have been reported with haloperidol. The risk of these events appears to increase with high doses, high plasma concentrations, in predisposed patients or with parenteral use, particularly intravenous administration.
- Haloperidol solution for injection is recommended for intramuscular administration only. However, if administered intravenously, continuous ECG monitoring must be performed for QTc interval prolongation and for ventricular arrhythmias.
- Caution is advised in patients with bradycardia, cardiac disease, family history of QTc prolongation or history of heavy alcohol
exposure. Caution is also required in patients with potentially high plasma concentrations.
- A baseline ECG is recommended before intramuscular dosing. During therapy, the need for ECG monitoring for QTc interval prolongation and for ventricular arrhythmias must be assessed in all patients, but continuous ECG monitoring is recommended for repeated intramuscular doses. ECG monitoring is recommended up to 6 hours after administration of Haloperidol solution for injection to patients for prophylaxis or treatment of postoperative nausea and vomiting. Whilst on therapy, it is recommended to reduce the dose if QTc is prolonged, but haloperidol must be discontinued if the QTc exceeds 500 ms.
- Electrolyte disturbances such as hypokalaemia and hypomagnesaemia increase the risk for ventricular arrhythmias and must be corrected before treatment with haloperidol is started. Therefore, baseline and periodic electrolyte monitoring is recommended.
- Tachycardia and hypotension (including orthostatic hypotension) have also been reported. Caution is recommended when haloperidol is administered to patients manifesting hypotension or orthostatic hypotension.
Cerebrovascular events:
- In randomised, placebo-controlled clinical studies in the dementia population, there was an approximately 3-fold increased risk of cerebrovascular adverse events with some atypical antipsychotics. Observational studies comparing the stroke rate in elderly patients exposed to any antipsychotic to the stroke rate in those not exposed to such medicinal products found an increased stroke rate among exposed patients. This increase may be higher with all butyrophenones, including haloperidol. The mechanism for this increased risk is not known.
- Haloperidol must be used with caution in patients with risk factors for stroke.
Neuroleptic malignant syndrome:
- Haloperidol has been associated with neuroleptic malignant syndrome: a rare idiosyncratic response characterized by hyperthermia, generalised muscle rigidity, autonomic instability, altered consciousness and increased serum creatine phosphokinase levels. Hyperthermia is often an early sign of this syndrome.
- Antipsychotic treatment must be withdrawn immediately and appropriate supportive therapy and careful monitoring instituted.
Tardive dyskinesia:
Tardive dyskinesia may appear in some patients on long-term therapy or after discontinuation of the medicinal product. The syndrome is mainly characterized by rhythmic involuntary movements of the tongue, face, mouth or jaw. The manifestations may be permanent in some patients. The syndrome may be masked when treatment is reinstituted, when the dose is increased.
or when a switch is made to a different antipsychotic. If signs and symptoms of tardive dyskinesia appear, the discontinuation of all antipsychotics, including haloperidol, must be considered.
Extrapyramidal symptoms:
- Extrapyramidal symptoms may occur (e.g. tremor, rigidity, hypersalivation, bradykinesia, akathisia, acute dystonia).
- The use of haloperidol has been associated with the development of akathisia, characterised by a subjectively unpleasant or distressing restlessness and need to move, often accompanied by an inability to sit or stand still. This is most likely to occur within the first few weeks of treatment. In patients who develop these symptoms, increasing the dose may be detrimental.
- Acute dystonia may occur during the first few days of treatment with haloperidol, but later onset as well as onset after dose increases has been reported. Dystonic symptoms can include, but are not limited to, torticollis, facial grimacing, trismus, tongue protrusion, and abnormal eye movements, including oculogyric crisis. Males and younger age groups are at higher risk of experiencing such reactions. Acute dystonia may necessitate stopping the medicinal product.
- Antiparkinson medicinal products of the anticholinergic type may be prescribed as required to manage extrapyramidal symptoms, but it is recommended that they are not prescribed routinely as a preventive measure. If concomitant treatment with an antiparkinson medicinal product is required, it may have to be continued after stopping haloperidol if its excretion is faster than that of haloperidol in order to avoid the development or aggravation of extrapyramidal symptoms. The possible increase in intraocular pressure must be considered when anticholinergic medicinal products, including antiparkinson medicinal products, are administered concomitantly with haloperidol.
Seizures/Convulsions:
It has been reported that seizures can be triggered by Haloperidol. Caution is advised in patients suffering from epilepsy and in conditions predisposing to seizures (e.g. alcohol withdrawal and brain damage).
Hepatobiliary concerns:
As haloperidol is metabolised by the liver, half the initial dose and caution is advised in patients with hepatic impairment.
Isolated cases of liver function abnormalities or hepatitis, most often cholestatic, have been reported.
Endocrine system concerns:
- Thyroxin may facilitate Haloperidol toxicity. Antipsychotic therapy in patients with hyperthyroidism must be used only with caution and must always be accompanied by therapy to achieve an euthyroid state.
- Hormonal effects of antipsychotic neuroleptic drugs include hyperprolactinaemia, which may cause galactorrhoea, gynaecomastia and oligo or amenorrhoea.
- Tissue culture studies suggest that cell growth in human breast tumours may be stimulated by prolactin.
- Caution is recommended in patients with relevant medical history. Haloperidol must be used with caution in patients with pre-existing hyperprolactinaemia and in patients with possible prolactin-dependent tumours.
Hypoglycaemia and syndrome of inappropriate antidiuretic hormone secretion have been reported with haloperidol.
Venous thromboembolism:
Cases of venous thromboembolism (VTE) have been reported with antipsychotic drugs. Since patients treated with antipsychotics often present with acquired risk factors for VTE, all possible risk factors for VTE should be identified before and during treatment with Haloperidol and preventive measures undertaken.
Treatment response and withdrawal:
- In schizophrenia, the response to antipsychotic treatment may be delayed.
If antipsychotics are withdrawn, recurrence of symptoms related to the underlying condition may not become apparent for several weeks or months.
There have been very rare reports of acute withdrawal symptoms (including nausea, vomiting and insomnia) after abrupt withdrawal of high doses of antipsychotics. Gradual withdrawal is advisable as a precautionary measure.
2- Patients with depression:
It is recommended that haloperidol is not used alone in patients in whom depression is predominant. It may be combined with antidepressants to treat those conditions in which depression and psychosis coexist.
3- Switch from mania to depression:
There is a risk in the treatment of manic episodes of bipolar disorder for patients to switch from mania to depression. Monitoring of patients for the switch to a depressive episode with the accompanying risks such as suicidal behaviour is important in order to intervene when such switches occur.
Poor metabolisers of CYP2D6:
Haloperidol should be used with caution in patients who are known poor metabolisers of cytochrome P450 (CYP) 2D6 and who
are coadministered a CYP3A4 inhibitor.
Drug Interactions:
Haloperidol is contraindicated in combination with medicinal products known to prolong the QT
•Class IA antiarrhythmics (e.g. disopyramide, quinidine).
• Class III antiarrhythmics (e.g. amiodarone, dofetilide, dronedarone, ibutilide,
Certain Antidepressants: citalopram. escitalopram
Certain antibiotics: azithromycin, clarithromycin, levofloxacin, erythromycin
Other antipsychotics: phenothiazine derivatives, pimozide, ziprasidone
Certain antifungals:pentamidine
Certain antimalarials: halofantrine
Certain gastrointestinal medicinal products: dolasetron
Certain medicinal products used in cancer: toremifene, vandetanib
other medicinal products: bepridil, methadone
2- Medicinal products that may increase haloperidol plasma concentrations:
CYP3A4 inhibitors: alprazolam, fluvoxamine, itraconazole, ketoconazole, Verapamil, voriconazole.
CYP2D6 inhibitors: bupropion, chlorpromazine, paroxetine, promethazine, sertraline, venlafaxine.
Combined CYP3A4 and CYP2D6 inhibitors: fluoxetine, ritonavir.
Uncertain mechanism: buspirone.
3- Medicinal products that may decrease haloperidol plasma concentrations:
enzyme inducers of CYP3A4 such as: Carbamazepine, phenobarbital, phenytoin, rifampicin.
4- Effect of haloperidol on other medicinal products:
- Haloperidol can increase the CNS depression produced by alcohol or CNS-depressant medicinal products
- Haloperidol may antagonise the action of adrenaline and other sympathomimetic medicinal products
- Haloperidol may antagonise the effect of levodopa and other dopamine agonists
- Haloperidol inhibits the metabolism of tricyclic antidepressants, thereby increasing plasma concentrations of these medicinal products.
USE IN PREGNANCY AND LACTATION:
It is preferable to avoid the use of haloperidol during pregnancy.
Haloperidol is excreted in human milk. A decision must be made whether to discontinue breastfeeding or to discontinue haloperidol therapy taking into account the benefit of breastfeeding for the child and the benefit of therapy for the woman.
Effects on ability to drive and use machines:
Haloperidol has a moderate influence on the ability to drive and use machines. Some degree of sedation or impairment of alertness may occur. Particularly with higher doses and at the start of treatment and may be potentiated by alcohol. It is recommended that patients be advised not to drive or operate machines during treatment, until their susceptibility is known.
PHARMACOKINETIC PROPERTIES:
Absorption: haloperidol is completely absorbed. Peak plasma concentrations of haloperidol are attained within 20 to 40 minutes.
Distribution: Mean haloperidol plasma protein binding in adults is approximately 88 to 92%.
Biotransformation:
Haloperidol is extensively metabolised in the liver. The main metabolic pathways of haloperidol in humans include glucuronidation, ketone reduction, oxidative N-dealkylation and formation of pyridinium metabolites. The metabolites of haloperidol are not considered to make a significant contribution to its activity; however, cannot be fully ruled out. The cytochrome P450 enzymes CYP3A4 and CYP2D6 are involved in haloperidol metabolism.
Inhibition or induction of CYP3A4, or inhibition of CYP2D6, may affect haloperidol metabolism. A decrease in CYP2D6 enzyme activity may result in increased haloperidol concentrations.
Elimination: The terminal elimination half-life of haloperidol is on average 21 hours after intramuscular administration.
After intravenous haloperidol administration, 21% of the dose was eliminated in the faeces and 33% in the urine. Less than 3% of the dose is excreted unchanged in the urine.
Overdose:
Symptoms and signs:
The manifestations of haloperidol overdose are an exaggeration of the known pharmacological effects and adverse reactions.
The most prominent symptoms are severe extrapyramidal reactions, hypotension and sedation. An extrapyramidal reaction is manifest by muscular rigidity and a generalised or localised tremor. Hypertension rather than hypotension is also possible.
In extreme cases, the patient would appear comatose with respiratory depression and hypotension that could be severe enough to produce a shock-like state. The risk of ventricular arrhythmias, possibly associated with QTc prolongation, must be considered.
Management:
There is no specific antidote. Treatment is supportive. Dialysis is not recommended in the treatment of overdose because it removes only very small amounts of haloperidol.
For comatose patients, a patent airway must be established by use of an oropharyngeal airway or endotracheal tube.
Respiratory depression may necessitate artificial respiration.
It is recommended that ECG and vital signs be monitored, and that monitoring continues until the ECG is normal. Treatment of severe arrhythmias with appropriate anti-arrhythmic measures is recommended.
Hypotension and circulatory collapse may be counteracted by use of intravenous fluids, plasma or concentrated albumin and vasopressor agents, such as dopamine or noradrenaline. Adrenaline must not be used because it might cause profound hypotension in the presence of haloperidol.
In cases of severe extrapyramidal reactions, parenteral administration of an antiparkinson medicinal product is recommended