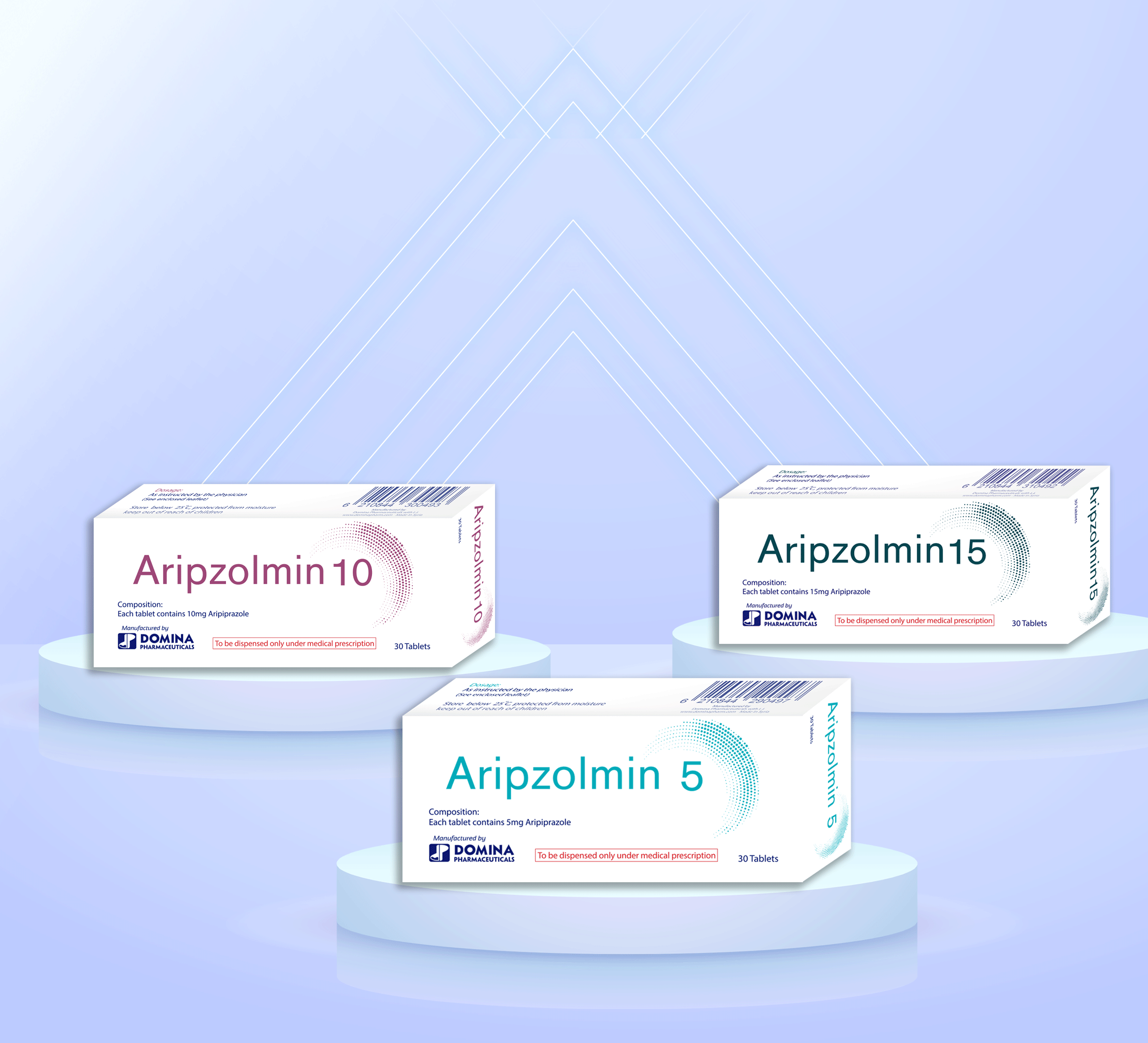
Composition:
Each tablet contains 5mg, 10mg, or 15mg Aripiprazole.
Mechanism Of Action:
The mechanism of action of aripiprazole in schizophrenia or bipolar mania, is unknown. However, the efficacy of aripiprazole could be mediated through a combination of partial agonist activity at D2 and 5-HT1A receptors and antagonist activity at 5-HT2A receptors. Aripiprazole exhibits high affinity for dopamine D2 and D3, serotonin 5-HT1A and 5-HT2A receptors.
Pharmacokinetics:
Absorption:
Aripiprazole is well absorbed after administration of the tablet, with peak plasma concentrations occurring within 3 hours to 5 hours; the absolute oral bioavailability of the tablet formulation is 87%. ARIPIPRAZOLE can be administered with or without food. Administration of a 15 mg ARIPIPRAZOLE Tablet with a standard high-fat meal did not significantly affect the Cmax or AUC of aripiprazole or its active metabolite.
Distribution: aripiprazole and its major metabolite are greater than 99% bound to serum proteins, primarily to albumin.
Metabolism And Elimination:
Following a single oral dose of (14C)-labeled aripiprazole, approximately 25% and 55% of the administered dose was recovered in the urine and feces, respectively. Less than 1% of unchanged aripiprazole was excreted in the urine and approximately 18% of the oral dose was recovered unchanged in the feces.
INDICATIONS:
ARIPIPRAZOLE is indicated for the treatment of:
- Schizophrenia .
- Acute Treatment of Manic and Mixed Episodes associated with Bipolar I Disorder.
- Adjunctive Treatment of Major Depressive Disorder .
- Irritability Associated with Autistic Disorder .
- Treatment of Tourette's Disorder.
CONTRAINDICATIONS:
ARIPIPRAZOLE is contraindicated in patients with a history of a hypersensitivity reaction to aripiprazole. Reactions have ranged from pruritus/urticaria to anaphylaxis.
DOSAGE AND ADMINISTRATION:
Schizophrenia:
- Adults:
The recommended starting and target dose for ARIPIPRAZOLE is 10 or 15 mg/day administered on a once-a-day schedule without regard to meals. ARIPIPRAZOLE has been systematically evaluated and shown to be effective in a dose range of 10 to 30 mg/day, when administered as the tablet formulation; however, doses higher than 10 or 15 mg/day were not more effective than 10 or 15 mg/day. Dosage increases should generally not be made before 2 weeks, the time needed to achieve steady-state .
Maintenance Treatment: Maintenance of efficacy in schizophrenia was demonstrated in a trial involving patients with schizophrenia who had been symptomatically stable on other antipsychotic medications for periods of 3 months or longer. These patients were discontinued from those medications and randomized to either ARIPIPRAZOLE 15 mg/day or placebo, and observed for relapse . Patients should be periodically reassessed to determine the continued need for maintenance treatment.
-Adolescents:
The recommended target dose of ARIPIPRAZOLE is 10 mg/day. Aripiprazole was studied in adolescent patients 13 to 17 years of age with schizophrenia at daily doses of 10 mg and 30 mg. The starting daily dose of the tablet formulation in these patients was 2 mg, which was titrated to 5 mg after 2 days and to the target dose of 10 mg after 2 additional days. Subsequent dose increases should be administered in 5 mg increments. The 30 mg/day dose was not shown to be more efficacious than the 10 mg/day dose. ARIPIPRAZOLE can be administered without regard to meals .Patients should be periodically reassessed to determine the need for maintenance treatment.
Switching From Other Antipsychotics:
There are no systematically collected data to specifically address switching patients with schizophrenia from other antipsychotics to ARIPIPRAZOLE or concerning concomitant administration with other antipsychotics. While immediate discontinuation of the previous antipsychotic treatment may be acceptable for some patients with schizophrenia, more gradual discontinuation may be most appropriate for others. In all cases, the period of overlapping antipsychotic administration should be minimized.
Bipolar I Disorder:
Acute Treatment Of Manic And Mixed Episodes:
- Adults: The recommended starting dose in adults is 15 mg given once daily as monotherapy and 10 mg to 15 mg given once daily as adjunctive therapy with lithium or valproate. ARIPIPRAZOLE can be given without regard to meals. The dose may be increased to 30 mg/day based on clinical response. The safety of doses above 30 mg/day has not been evaluated in clinical trials.
- Pediatrics: The recommended starting dose in pediatric patients (10 to 17 years) as monotherapy is 2 mg/day, with titration to 5 mg/day after 2 days, and a target dose of 10 mg/day after 2 additional days. Recommended dosing as adjunctive therapy to lithium or valproate is the same. Subsequent dose increases, if needed, should be administered in 5 mg/day increments. ARIPIPRAZOLE can be given without regard to meals.
Adjunctive Treatment Of Major Depressive Disorder:
Adults:
The recommended starting dose for ARIPIPRAZOLE as adjunctive treatment for patients already taking an antidepressant is 2 to 5 mg/day. The recommended dosage range is 2 to 15 mg/day. Dosage adjustments of up to 5 mg/day should occur gradually, at intervals of no less than 1 week. Patients should be periodically reassessed to determine the continued need for maintenance treatment.
Irritability Associated With Autistic Disorder:
Pediatric Patients (6 to 17 years):
The recommended dosage range for the treatment of pediatric patients with irritability associated with autistic disorder is 5 to 15 mg/day.
Dosing should be initiated at 2 mg/day. The dose should be increased to 5 mg/day, with subsequent increases to 10 or 15 mg/day if needed. Dose adjustments of up to 5 mg/day should occur gradually, at intervals of no less than 1 week. Patients should be periodically reassessed to determine the continued need for maintenance treatment.
Tourette's Disorder:
Pediatric Patients (6 to 18 years):
The recommended dosage range for Tourette's Disorder is 5 to 20 mg/day.
For patients weighing less than 50 kg, dosing should be initiated at 2 mg/day with a target dose of 5 mg/day after 2 days. The dose can be increased to 10 mg/day in patients who do not achieve optimal control of tics. Dosage adjustments should occur gradually at intervals of no less than 1 week.
For patients weighing 50 kg or more, dosing should be initiated at 2 mg/day for 2 days, and then increased to 5 mg/day for 5 days, with a target dose of 10 mg/day on day 8. The dose can be increased up to 20 mg/day for patients who do not achieve optimal control of tics. Dosage adjustments should occur gradually in increments of 5 mg/day at intervals of no less than 1 week.Patients should be periodically reassessed to determine the continued need for maintenance treatment.
SIDE EFFECTS:
nausea, vomiting, constipation, headache, dizziness, akathisia, anxiety, insomnia, and restlessness, somnolence, extrapyramidal disorder, fatigue, increased appetite, nasopharyngitis, and weight increased, Sedation, Tremor, Blurred Vision, Abdominal Discomfort, Gastrointestinal Disorders, Salivary Hypersecretion, Pyrexia, Irritability , Extrapyramidal Disorder, Dystonia, Rash, Arthralgia, Myalgia, Tachycardia.
DRUG INTERACTIONS:
Strong CYP3A4 Inhibitors (e.g., itraconazole, clarithromycin) or strong CYP2D6 inhibitors (e.g., quinidine, fluoxetine, paroxetine):
increased the exposure of aripiprazole compared to the use of ARIPIPRAZOLE alone. reduce the ARIPIPRAZOLE dosage.
Strong CYP3A4 Inducers (e.g., carbamazepine, rifampin):
decreased the exposure of aripiprazole compared to the use of ARIPIPRAZOLE alone. increasing the ARIPIPRAZOLE dosage.
Antihypertensive Drugs:
aripiprazole has the potential to enhance the effect of certain antihypertensive agents. Monitor blood pressure and adjust dose accordingly.
Benzodiazepines (e.g., lorazepam):
The intensity of sedation was greater with the combination of oral aripiprazole and lorazepam as compared to that observed with aripiprazole alone. The orthostatic hypotension observed was greater with the combination as compared to that observed with lorazepam alone.Monitor sedation and blood pressure. Adjust dose accordingly.
No dosage adjustment is necessary for substrates of CYP2D6 (e.g., dextromethorphan, fluoxetine, paroxetine, or venlafaxine), CYP2C9 (e.g., warfarin), CYP2C19 (e.g., omeprazole, warfarin, escitalopram), or CYP3A4 (e.g., dextromethorphan) when co-administered with ARIPIPRAZOLE. Additionally, no dosage adjustment is necessary for valproate, lithium, lamotrigine, lorazepam, or sertraline when co-administered with ARIPIPRAZOLE.
PRECAUTIONS:
Increased Mortality In Elderly Patients With Dementia-Related Psychosis:
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. ARIPIPRAZOLE (aripiprazole) is not approved for the treatment of patients with dementia-related psychosis.
The safety and efficacy of ARIPIPRAZOLE in the treatment of patients with psychosis associated with dementia have not been established. If the prescriber elects to treat such patients with ARIPIPRAZOLE, assess for the emergence of difficulty swallowing or excessive somnolence, which could predispose to accidental injury or aspiration.
Cerebrovascular Adverse Events, Including Stroke:
There was an increased incidence of cerebrovascular adverse events (e.g., stroke, transient ischemic attack), including fatalities, in ARIPIPRAZOLE -treated patients.
Suicidal Thoughts And Behaviors In Children, Adolescents, And Young Adults:
Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs.
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases.
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania, have been reported in adult and pediatric patients being treated with antidepressants for MDD as well as for other indications, both psychiatric and nonpsychiatric.
Screening Patients For Bipolar Disorder:
A major depressive episode may be the initial presentation of bipolar disorder. It is generally believed (though not established in controlled trials) that treating such an episode with an antidepressant alone may increase the likelihood of precipitation of a mixed/manic episode in patients at risk for bipolar disorder.
Neuroleptic Malignant Syndrome (NMS):
A potentially fatal symptom complex sometimes referred to as Neuroleptic Malignant Syndrome (NMS) may occur with administration of antipsychotic drugs, including ARIPIPRAZOLE.
Tardive Dyskinesia:
A syndrome of potentially irreversible, involuntary, dyskinetic movements may develop in patients treated with antipsychotic drugs. Although the prevalence of the syndrome appears to be highest among the elderly, especially elderly women, it is impossible to rely upon prevalence estimates to predict, at the inception of antipsychotic treatment, which patients are likely to develop the syndrome. Whether antipsychotic drug products differ in their potential to cause tardive dyskinesia is unknown.
Metabolic Changes:
Atypical antipsychotic drugs have been associated with metabolic changes that include hyperglycemia/diabetes mellitus, dyslipidemia, and body weight gain. While all drugs in the class have been shown to produce some metabolic changes, each drug has its own specific risk profile.
Hyperglycemia/Diabetes Mellitus:
Hyperglycemia, in some cases extreme and associated with ketoacidosis or coma or death, has been reported in patients treated with atypical antipsychotics. There have been reports of hyperglycemia in patients treated with ARIPIPRAZOLE.
Orthostatic Hypotension:
ARIPIPRAZOLE may cause orthostatic hypotension, perhaps due to its α1-adrenergic receptor antagonism.
ARIPIPRAZOLE should be used with caution in patients with known cardiovascular disease (history of myocardial infarction or ischemic heart disease, heart failure or conduction abnormalities), cerebrovascular disease, or conditions which would predispose patients to hypotension (dehydration, hypovolemia, and treatment with antihypertensive medications).
Leukopenia, Neutropenia, And Agranulocytosis:
In clinical trials and/or postmarketing experience, events of leukopenia and neutropenia have been reported temporally related to antipsychotic agents, including ARIPIPRAZOLE. Agranulocytosis has also been reported.
Seizures/Convulsions:
As with other antipsychotic drugs, ARIPIPRAZOLE should be used cautiously in patients with a history of seizures or with conditions that lower the seizure threshold. Conditions that lower the seizure threshold may be more prevalent in a population of 65 years or older.
Potential For Cognitive And Motor Impairment:
ARIPIPRAZOLE, like other antipsychotics, may have the potential to impair judgment, thinking, or motor skills. For example, in short-term, somnolence (including sedation) was reported .
Body Temperature Regulation:
Disruption of the body's ability to reduce core body temperature has been attributed to antipsychotic agents. Appropriate care is advised when prescribing ARIPIPRAZOLE for patients who will be experiencing conditions which may contribute to an elevation in core body temperature, (e.g., exercising strenuously, exposure to extreme heat, receiving concomitant medication with anticholinergic activity, or being subject to dehydration).
Suicide:
The possibility of a suicide attempt is inherent in psychotic illnesses, bipolar disorder, and major depressive disorder, and close supervision of high-risk patients should accompany drug therapy. Prescriptions for ARIPIPRAZOLE should be written for the smallest quantity consistent with good patient management in order to reduce the risk of overdose.
Dysphagia:
Esophageal dysmotility and aspiration have been associated with antipsychotic drug use, including ARIPIPRAZOLE. Aspiration pneumonia is a common cause of morbidity and mortality in elderly patients, in particular those with advanced Alzheimer's dementia. ARIPIPRAZOLE and other antipsychotic drugs should be used cautiously in patients at risk for aspiration pneumonia.
Pregnancy: Pregnancy Category C
Administer ARIPIPRAZOLE during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nursing Mothers: ARIPIPRAZOLE is present in human breast milk. Because of the potential for serious adverse reactions in nursing infants from ARIPIPRAZOLE, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use: Safety and effectiveness in pediatric patients with major depressive disorder or agitation associated with schizophrenia or bipolar mania have not been established.
Geriatric Use: No dosage adjustment is recommended for elderly patients.
Hepatic And Renal Impairment: No dosage adjustment for ARIPIPRAZOLE is required on the basis of a patient's hepatic function (mild to severe hepatic impairment ) , or renal function (mild to severe renal impairment, glomerular filtration rate between 15 and 90 mL/minute).
OVERDOSE:
Common adverse reactions (reported in at least 5% of all overdose cases) reported with oral ARIPIPRAZOLE overdosage (alone or in combination with other substances) include vomiting, somnolence, and tremor. Other clinically important signs and symptoms observed in one or more patients with ARIPIPRAZOLE overdoses (alone or with other substances) include acidosis, aggression, aspartate aminotransferase increased, atrial fibrillation, bradycardia, coma, confusional state, convulsion, blood creatine phosphokinase increased, depressed level of consciousness, hypertension, hypokalemia, hypotension, lethargy, loss of consciousness, QRS complex prolonged, QT prolonged, pneumonia aspiration, respiratory arrest, status epilepticus, and tachycardia.
Management Of Overdosage:
No specific information is available on the treatment of overdose with ABILIFY. An electrocardiogram should be obtained in case of overdosage and if QT interval prolongation is present, cardiac monitoring should be instituted. Otherwise, management of overdose should concentrate on supportive therapy, maintaining an adequate airway, oxygenation and ventilation, and management of symptoms. Close medical supervision and monitoring should continue until the patient recovers.